Interview with Brendan Martin by Anna Betz for Enlivening Edge Magazine
Part 1 of this 3-part article is here. Part 2 of this 3-part article is here.
What is your success in having conversations with leaders to enable them to see more possibilities? Is there ever a no-no situation?
We don’t have a formula. A lot of it is gut feeling. There isn’t a single organisation that is homogenous in this respect.
Typically the particular focus of attention of different people in the organisation varies. We often work with a clinician in a leadership position who is very much driven by the potential they see for improving care and job satisfaction. In order to get traction within their organization they also have to demonstrate the potential financial benefits.
We try to collaborate with them and support them in having the kind of conversations they need to have within their organization to get support.
By definition we are working with organisations within social care and the National Health Service who want to pioneer this approach. We can assume that they are most ready in their mindset to be innovative, to accept risk taking and to break new ground.
However, this doesn’t necessarily mean they understand the nature and scale of organizational change required to create the supportive and enabling environment for self-organized team work.
The bigger question for us is whether we need people to sign up for a whole programme of change starting with inspiration, decision-making about a journey, and ending with a completely radically changed and completely restructured organization.
The 3 things we bring:
1. We say we are here to facilitate your organisational learning about what it takes if you agree with us about basic values and intention, and we agree broadly about what you want to achieve in terms of person-centred care, building a trusting environment for professionals to do their job in an autonomous way.
If we get an agreement about that, there will be a lot more detail further along the journey as we don’t know enough about a particular organisation. We offer to identify these details with the organisation and move forward step by step as the challenges arise.
The focus is always on building a trusting relationship so they trust what will emerge for them at the right time in their organisation. It is important to keep the dialogue going on how to deal with challenges as they arise.

2.We operate in two ways: Sometimes people ask us for very discrete services to help them with this or that bit of organisational change that is in keeping with our values and which we have the expertise and capacity to help them with.
When we can, and when it is appropriate, we offer a one-off support, but broadly we much prefer to build longterm relationships to co-create longterm solutions where we play a facilitative role. We bring in expertise, experience. and knowledge about what made Buurtzorg and other organisations succeed in the Netherlands. We bring in a growing body of knowledge and understanding about the experience in Britain. How to bring the Buurtzorg way into Britain has completely transformed from 1 or 2 years ago.
 3.We bring experience and skills in facilitating discussions and processes that are needed within organisations to create the new organisational environment for this approach to flourish.We much prefer, and increasingly are requiring from our own point of view, that the people we work with want to go on that collaborative co-creative pathway with us. We do that with humility, knowing that we don’t understand all the pressures people are under which includes emotional, psychological or clinical pressures.
3.We bring experience and skills in facilitating discussions and processes that are needed within organisations to create the new organisational environment for this approach to flourish.We much prefer, and increasingly are requiring from our own point of view, that the people we work with want to go on that collaborative co-creative pathway with us. We do that with humility, knowing that we don’t understand all the pressures people are under which includes emotional, psychological or clinical pressures.
There are also technical issues that they know a lot more about. We have to be open to collaboration to find co-creative solutions.
What kinds of relationships do you want?
We would rather work with a smaller number of organisations that present themselves to us than working with a large number of organisations that are not really open to change mindsets. You cannot create person-centred care provided by self-managing local teams within organisations that maintain all their old mindsets and hierarchical structures.
Creating solutions and making promises based on false ideas and expectations isn’t sustainable.
We openly talk about the pathway organisations will be on and make it clear that we don’t know how long they are going to go on this journey, what that road is going to look like in their particular case, and what the challenges will be, but we can tell them that they can’t have it both ways.
When you are working with organisations, do you address their pay structures and their job descriptions?
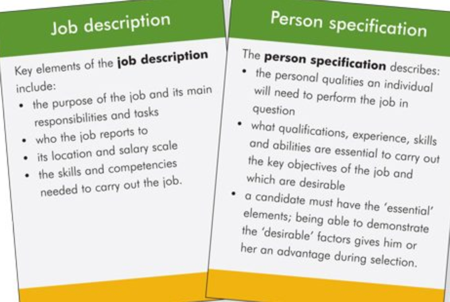
When it comes to job descriptions, even when you get started with a test-and-learn project, you have to draw up job descriptions in a different way because people working in those test-and-learn teams are going to work in a different way. Therefore the conventional job description isn’t suitable for that purpose. We support organisations in looking at the job descriptions they need for members of self-sustaining teams and for other people involved with them.
The system being what it is also involves reaching compromises that have to be made sometimes if you are going to get started at all. Unless you get going and create a practical experience from which learning can grow, you never grow the learning at all. You have to find ways to connect job descriptions, rule books, and the framework for a self-organised team.
How do you measure the impact of the new teams, and what methods of assessing benefit would you recommend?
Most of the projects we are working in are being externally evaluated, but in different ways. Some are asking the question “Can the Buurtzorg model work here?” We think that is the wrong question because we believe the fundamental ethos of Buurtzorg is universal; humanity knows no geographical boundaries so neither should ‘humanity above bureaucracy’.
Also, unless there are organisational and systemic changes to enable it to work at scale, then the answer is likely to be “No it doesn’t work”–because it won’t! So we prefer the question “How can it work here?” because that means we are testing and learning about what needs to change to enable it to work.
Are the sorts of staff people who work well as part of the new teams different from those working in more traditional areas?
Fundamentally I would say any professional nurse or caregiver with the right values and vocational commitment will succeed in a self-organised team. But it’s also true that you need the right attitude to taking responsibility, working with diversity, listening well to each other while taking ownership of your own opinion, and so on. Those kinds of attitudes and skills are important, and without them you can struggle in a self-organised team. We need to be honest and admit it’s not for everyone.

How do you think this approach could be of value to acute and residential settings?
Buurtzorg in the Netherlands is already showing how it works in some residential settings. I see no reason why the fundamentals would not work in acute settings too, but no doubt there are some specific aspects that will need to be considered and learnt about through experience.
As the Buurtzorg approach links very closely with local communities, are there types of communities that work better than others and get more benefit from the team? What do you do to assess or develop the community to host the team?
It’s interesting that the teams in two neighbouring south London boroughs have found that one of them has a stronger community and voluntary base than the other, and that is making a difference. That is a challenge for the teams themselves rather than for us.
Our role is to support them and their organisations to enable them to solve whatever problems they have. I’m very confident that with the right organisational support teams will not only mobilise local voluntary and community resources well, but help to develop them.
 Brendan Martin is founder and Managing Director of Public World and Buurtzorg Britain & Ireland, which work to support better care and services and more fun at work through self-managed teams in high trust organisations. www.buurtzorg.org.uk
Brendan Martin is founder and Managing Director of Public World and Buurtzorg Britain & Ireland, which work to support better care and services and more fun at work through self-managed teams in high trust organisations. www.buurtzorg.org.uk
 Anna’s background is in Health and Social Care with training in Herbal Medicine, Socialwork, Mindfulness Practice, Transparent Communication, and Systemic Family Therapy. She practices a pro-active evolutionary approach to Health and Wellbeing and leads on projects in the UK National Health Service using Mindfulness and diet for people suffering from chronic inflammatory diseases like diabetes and dementia. Her passion for building thriving and sustainable communities inspired her to co-found the HealthCommonsHub. She feels at home in places where individual, communal, organisational, and social evolution meet, and where people support each other in becoming whole and feel enlivened.
Anna’s background is in Health and Social Care with training in Herbal Medicine, Socialwork, Mindfulness Practice, Transparent Communication, and Systemic Family Therapy. She practices a pro-active evolutionary approach to Health and Wellbeing and leads on projects in the UK National Health Service using Mindfulness and diet for people suffering from chronic inflammatory diseases like diabetes and dementia. Her passion for building thriving and sustainable communities inspired her to co-found the HealthCommonsHub. She feels at home in places where individual, communal, organisational, and social evolution meet, and where people support each other in becoming whole and feel enlivened.





Interesting 3 part article. Where can I find more about the specifics of Buurtzorg – eg, which type of staff make up the team, what is the staff to patient ratio, where does the GP fit in, what impact has it had on GP input, what impact on other services, what arrangements for other services to be more responsive, etc? I am an advocate of the Alaskan Nuka system, which operates from similar small team principles to Buurtzorg, only at primary care team level. The bottom line with Nuka is that it requires more staff and quicker access to more services, eg fewer patients per GP wte and real-time access to a wide range of extended services. What is the bottom line for Buurtzorg?
Dear Maxine,
Thank you for your important questions.
I dont have sufficient detail to answer your questions properly. Hopefully Brendan and/or Jos will address your questions.
In the meantime I found this article which may give you some idea of numbers and impact of the Neighbourhood Nursing teams with feedback from GPs and patients.
https://bmjopen.bmj.com/content/bmjopen/8/6/e021931.full.pdf
“The intervention of interest was the new team, known as the neighbourhood nursing (NN) team, who worked to the adapted Buurtzorg model still within a larger bureaucratic organisation. The first three members of the team, with the coach, were recruited and started visiting patients in November 2016. The role of the coach was to facilitate the team to be self-managing. The team visited patients who were registered with one of three general practices and lived within a 20 min walk of their office in a socioeconomically deprived area of inner London.
The team recruited new members throughout the first 6months until there were nine at which point they split into two teams, one covering a new area. As a self-managing team they made all operational decisions in weekly meetings conducted using Buurtzorg principles, including voting.
Their employing NHS Trust had a DN service of around 200 nurses and healthcare assistant
posts and at the time of the implementation a vacancy rate of 40%. The DN service was organised into teams each with a senior nurse. Each of these senior nurses reported to locality manager who in turn reported to another level in the organisation, which was only one of a number of divisions in the larger organisation.”
Some other resources you may find useful:
For figures:
https://www.england.nhs.uk/6cs/wp-content/uploads/sites/25/2015/04/implementing-buurtzorg-principles.pdf
https://www.nursingtimes.net/news/community/london-trust-to-roll-out-buurtzorg-community-nursing-model/7022833.article