By Anna Betz for Enlivening Edge Magazine
The keyword for the next economic, political, social, and medical model is “community.”
Our present culture is wasteful and inefficient. Many people feel alienated from their own soul, from their work, from each other, and from nature. We are experiencing a state of “systemic inflammation” that is perfectly mirrored in the drastically increasing number of chronic inflammatory diseases like obesity, heart problems, diabetes, arthritis, and dementia amongst others. Together they could–and probably will–crumble our health systems, unless we wake up to another way of doing medicine that makes us all feel more engaged, enlivened, and responsible.
Such a way of doing medicine, in which there is no waste of human potential and creativity requires re-organising healthcare from hierarchical to non-hierarchical organisations. This way of organizing which creates soulful workplaces where everyone’s talents are nurtured and their deepest aspirations are honoured is also known as Teal.[1]
Charles Eisenstein reminded us recently “We have arrived at a point where we source very little from our local communities. We can pretend we don’t need them, as we can buy food, shelter, clothing, and entertainment online from faraway places. Due to the distance and disconnection, we can ignore the conditions under which those goods are being produced.”[2]
What is the nature of social distance and disconnection that lets us ignore conditions under which our health as a good is produced? What is the meaning of community, and how can it be the future of medicine and our health as commons? Those two inter-related questions are at the heart of my enquiry.
Charles Eisenstein defines a community as a group of people bound together by gifts and stories, people who live in service of each other and the larger community. In a community people rely on each other. Gifts create ties and connections; we accept that we need each other, and we know deep down that being generous with our gifts will keep us safe.
When we feel as a community, we realize deeply that the wellbeing of another is our own wellbeing, and we realize the fortune and misfortune of another is our own. We can no longer ignore the needs of another when we realize they are part of us. Acknowledging the interconnectedness of our behaviour at every moment makes us act as a caring community.
A community model of doing medicine is not a one-way model where the professional has all the expert knowledge and tells the patient what to do. When medicine returns to the people, the role of professionals will be teachers who help patients discover their innate knowledge and wisdom, and who help them apply it in their everyday life to create conditions for health and wholeness. Doctors will learn from patients and feel inspired by the patient’s knowledge as much as the other way around. The title “doctor” is actually a Latin-derived word referring to anyone who is recognized as having acquired sufficient knowledge in a subject to be a teacher of the subject.
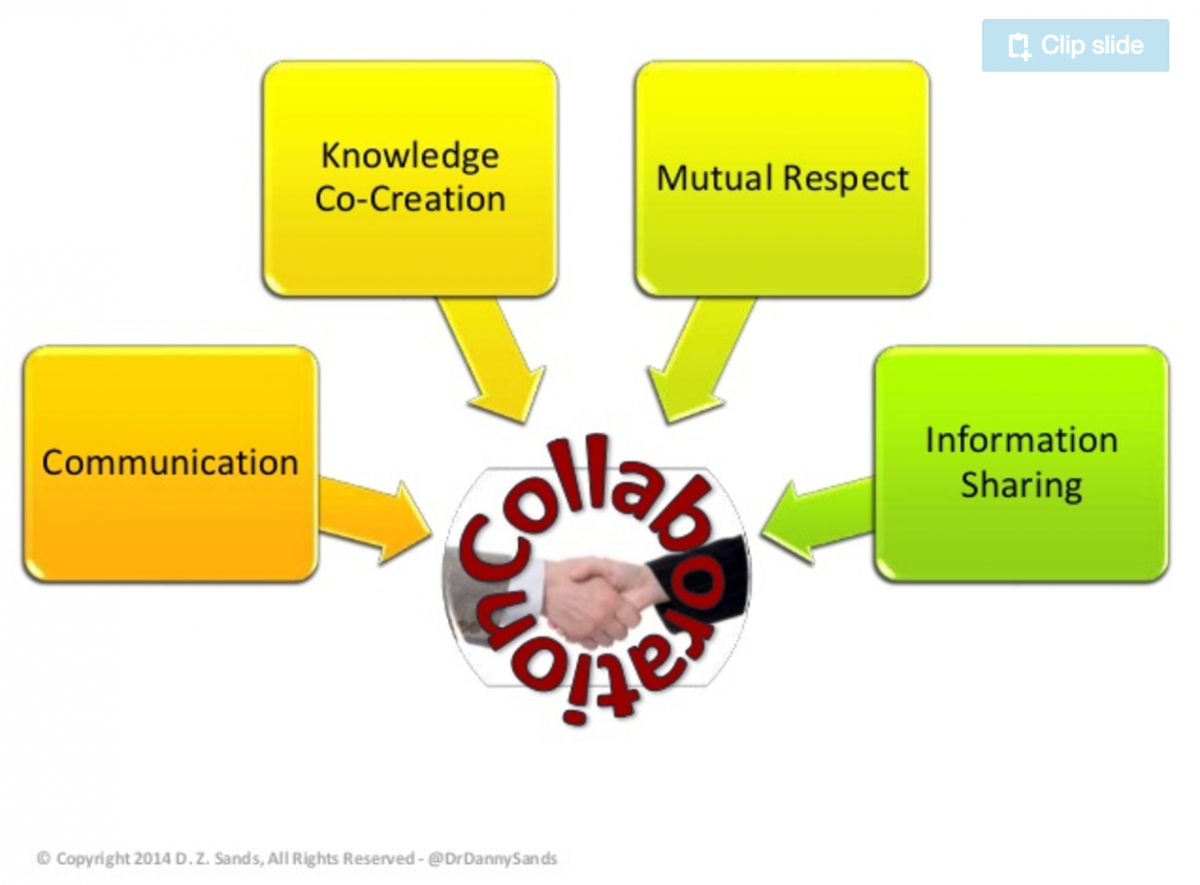
Collaboration in the community model can look like this[3]:
Returning medicine to the people means re-skilling ourselves in working with nature rather than trying to control it, thus enabling people to notice imbalances and symptoms before they become problems. It also means re-skilling everyone in using food as medicine and making lifestyle changes that bring us back into balance.
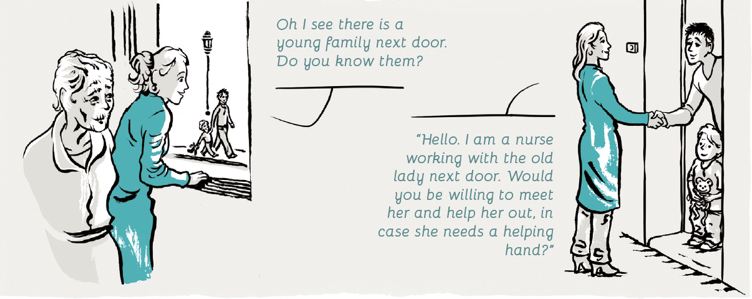
Clearly, that returning and re-skilling is a challenge, and “social prescribing” can be part of the answer. “Social prescribing is a way of linking patients in primary care with sources of support within the community. It provides GP’s [General Practice Doctors] with a non-medical-referral option that can operate alongside existing treatments to improve health and well-being.”[4]
Michael Dixon, National Clinical Lead for Social Prescription (National Health Service of England) believes “the answer to this challenge will be the social prescribing model which will begin to support the communal fabric of health and wellbeing.” He believes that “in subtle ways it will be helping general practices to make better use of their registered list to reframe themselves as hubs of local health development”. Although he claims that “the re-invention of the NHS won’t happen from the top down, and morale and purpose have to be restored at every level”, he does not talk about the kind of organisational structures that could support such a re-invention of the NHS.[5]
What kind of organisational structures would be dynamic enough to support a model of community and cooperative medicine that seeks to achieve active involvement by patients, professionals, care givers, and all others across the continuum of care, on all issues related to an individual’s health?
Could community perspectives and the patient’s voice regarding such things as treatments, clinical trials, and other domains traditionally belonging to a highly specialised science, have a real impact? Will a community be able to change inadequate or harmful medical, healthcare, and pharmaceutical practices, based on patient experience and evidence?
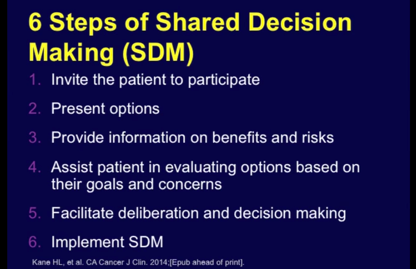
“Community and cooperative medicine” is an ethical approach to care that also holds promise to improve outcomes, reduce medical errors, increase patient satisfaction, and improve the cost of care. Such medicine relies much on participatory action research, community healthcare, participatory healthcare, and the anthropology of health. In this video Dr Daniel Z. Sands from Harvard Medical School shares his insights and gives good practical examples of an approach he calls “participatory medicine”.[6]
In the illustrated version of his book Reinventing Organizations, Frederic Laloux uses a metaphor from nature to illuminate how we would treat one another in a world where everyone matters and where we listen to what matters. “A fern or a mushroom growing next to a tree might not reach as high as the tree, but that is not the point. Through a complex collaboration involving exchanges of nutrients, moisture, and shade, the mushroom, fern, and tree don’t compete as much as they cooperate to grow into the biggest and healthiest versions of themselves.”[7]
It’s the same in Teal organizations and Teal-inspired healthcare: the point is not to make everyone equal; it is to allow employees, patients and communities to grow into the strongest next versions of themselves.
Source: Reinventing Organizations: An Illustrated Invitation to Join the Conversation on Next-Stage Organizations, by Frederic Laloux
[1] Frederic Laloux: http://www.strategy-business.com/article/00344?gko=10921
[2] https://youtu.be/lnQGSjDMnEc
[3] http://www.slideshare.net/dzsands/patient-care-as-collaboration Slide number 12. Daniel Z. Sands, MD, Speaker, consultant, thought leader, PCP @ intersection of healthcare, IT, & biz. Co-Founder, @S4PM. CMO
[4] Evidence to inform the commissioning of social prescribing, by University of York. https://www.york.ac.uk/media/crd/Ev%20briefing_social_prescribing.pdf
[5] https://www.collegeofmedicine.org.uk/wp-content/uploads/2016/12/Saving-the-NHS-by-Michael-Dixon.pdf
[6] The image just below is from time stamp 13:05 of this video https://youtu.be/q7I62IxRHRg from Dr. Sands.
[7] Reinventing Organizations: An Illustrated Invitation to Join the Conversation on Next-Stage Organizations, by Frederic Laloux. https://www.amazon.com/Reinventing-Organizations-Illustrated-Invitation-Conversation/dp/2960133552/
Anna’s background is in Health and Social Care with training in Herbal Medicine, Socialwork, Mindfulness Practice, Transparent Communication, and Systemic Family Therapy. She practices a pro-active evolutionary approach to Health and Wellbeing and leads on projects in the UK National Health Service using Mindfulness and diet for people suffering from chronic inflammatory diseases like diabetes and dementia. Her passion for building thriving and sustainable communities inspired her to co-found the HealthCommonsHub. She feels at home in places where individual, communal, organisational, and social evolution meet, and where people support each other in becoming whole and feel enlivened.